Tanning Beds Skin Cancer and Aging Skin Risks
In Addition to Aging Your Skin Prematurely, Do You Know the Dangers of Tanning Beds?
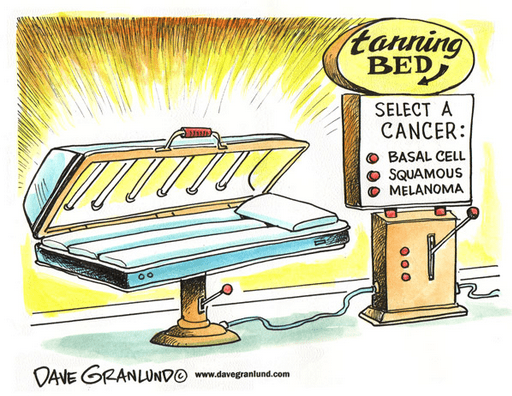
The end of winter to spring season is the time of year when we start to show more skin and begin working on getting a golden tan before vacation. Don’t be lured in to the tanning salon to get the golden glow! The World Health Organization has declared indoor tanning devices to be cancer-causing agents that are in the same category as tobacco. Studies have found a 59% increase in the risk of melanoma in those who have been exposed to UV radiation from indoor tanning.
To date, more than 30 states restrict access to indoor tanning equipment either through banning their use by minors or requiring parental consent. The American Academy of Dermatology Association (AADA) opposes indoor tanning and supports a ban on the production and sale of indoor tanning equipment for non-medical purposes.The AADA also supports the World Health Organization recommendation that minors should not use indoor tanning equipment. Unless and until the Food and Drug Administration bans the sale and use of indoor tanning equipment for non-medical purposes, the AADA supports restrictions for indoor tanning facilities, including: No person or facility should advertise the use of any UVA or UVB tanning device using wording such as “safe,” “safe tanning,” “no harmful rays,” “no adverse effect,” or similar wording or concepts.
Risk factors
- Exposure to natural and artificial ultraviolet (UV) light is a risk factor for all types of skin cancer.5
- Avoiding this risk factor alone could prevent more than 3 million cases of skin cancer every year.14
- More people develop skin cancer because of tanning than develop lung cancer because of smoking.17
- Increasing intermittent sun exposure in childhood and during one’s lifetime is associated with an increased risk of squamous cell carcinoma, basal cell carcinoma and melanoma.18
- Sustaining five or more blistering sunburns between ages 15 and 20 increases one’s melanoma risk by 80 percent and nonmelanoma skin cancer risk by 68 percent.19
- In 2010, new research found that daily sunscreen use cut the incidence of melanoma, the deadliest form of skin cancer, in half.20
- Exposure to tanning beds increases the risk of melanoma, especially in women 45 and younger.21
- In females 15 to 29 years old, the torso/trunk is the most common location for developing melanoma, which may be due to high-risk tanning behaviors.10,22
- Risk factors for all types of skin cancer include skin that burns easily; blond or red hair; a history of excessive sun exposure, including sunburns; tanning bed use; immune system-suppressing diseases or treatments; and a history of skin cancer.5
- People with more than 50 moles, atypical moles, or large moles are at an increased risk of developing melanoma, as are those with light skin and freckles, and those with a personal or family history of melanoma.5,23
- Melanoma survivors have an approximately nine-fold increased risk of developing another melanoma compared to the general population.24
- Men and women with a history of nonmelanoma skin cancer are at a higher risk of developing melanoma than people without a nonmelanoma skin cancer history.25
- Women with a history of nonmelanoma skin cancer are at a higher risk of developing leukemia, breast, kidney and lung cancers, and men with a history of nonmelanoma skin cancer are at a higher risk of developing prostate cancer. 25
 Prevention and detection
Prevention and detection
- Because exposure to UV light is the most preventable risk factor for all skin cancers14, the American Academy of Dermatology encourages everyone to protect their skin from the sun’s harmful UV rays by seeking shade, wearing protective clothing and using a sunscreen with a Sun Protection Factor of 30 or higher.
- Because severe sunburns during childhood may increase one’s risk of melanoma, children should be especially protected from the sun.5
- People should not use tanning beds or sun lamps, which are sources of artificial UV radiation that may cause skin cancer.5
- Skin cancer warning signs include changes in size, shape or color of a mole or other skin lesion, the appearance of a new growth on the skin, or a sore that doesn’t heal. If you notice any spots on your skin that are different from the others, or anything changing, itching or bleeding, the American Academy of Dermatology recommends that you make an appointment with a board-certified dermatologist.
- The American Academy of Dermatology encourages everyone to perform skin self-exams to check for signs of skin cancer and get a skin exam from a doctor. A dermatologist can make individual recommendations as to how often a person needs these exams based on risk factors, including skin type, history of sun exposure and family history.
- Individuals with a history of melanoma should have a full-body exam by a board-certified dermatologist at least annually and perform regular self-exams to check for new and changing moles.26
 Make an appointment for a full body skin cancer screening with our board-certified dermatology team today! Skin cancer screenings saves lives.
Make an appointment for a full body skin cancer screening with our board-certified dermatology team today! Skin cancer screenings saves lives.
Call 240-482-2555 for an appointment in Chevy Chase, Maryland, and 301-345-7375 for an appointment in Greenbelt, Maryland.